hankyoreh
Links to other country sites 다른 나라 사이트 링크
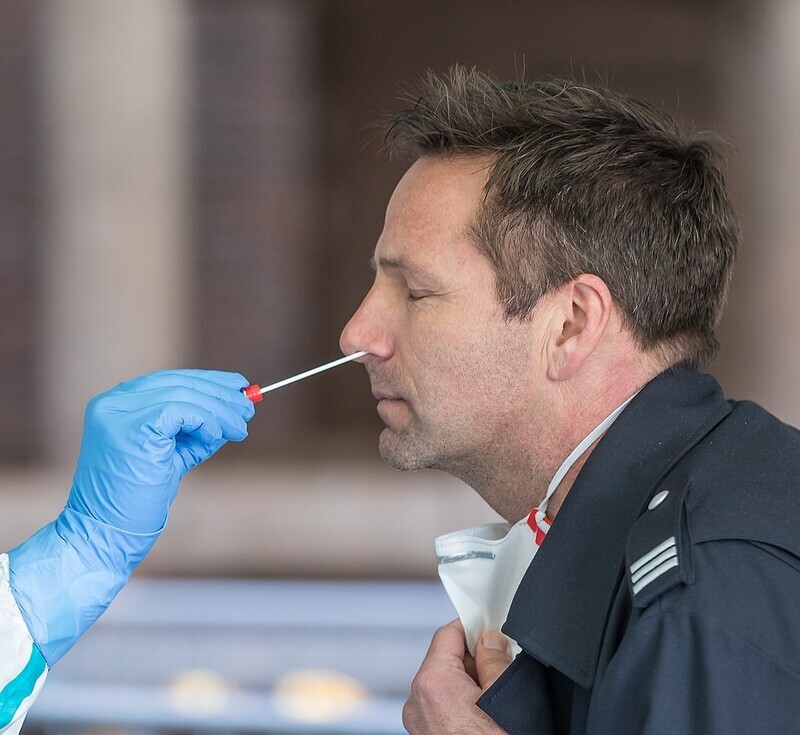
The science behind why COVID-19 affects all of us so differently

Some people who catch COVID-19 experience no symptoms at all while others suffer from symptoms so severe that they require hospitalization and intensive care. Others even continue to suffer from symptoms months after recovering from the initial infection. Why is it that symptoms vary so widely among people infected with the same virus?
The most decisive factor in serious symptoms? Age.Experts cite age as the most important factor in determining the severity of symptoms. As people get older, their immune system ages as well.
“As a child grows older, the immune system is stimulated by various pathogens and is completed in adolescence,” says Joo Chul-hyun, a professor of microbiology at the University of Ulsan College of Medicine. “From the age of 60 onward, the function [of the immune system] gradually begins to decline.” This is why health authorities classify people over the age of 60 as a high-risk group.
Children, on the other hand, rarely have severe symptoms. The reason has not been clearly identified, but scientists generally believe it is because children’s innate immune system, which they inherit genetically, responds quickly. Since the immune system reacts sensitively to even the most insignificant pathogen penetration in the bodies of children, germs or bacteria are more likely to lose steam before a virus can reach deep within the body.
Another factor is that the receptor protein (ACE2) gene of cells required for COVID-19 infection is less present in children. Other hypotheses as to why children have milder symptoms include the facts that they have healthier vascular and coagulation systems and healthier ciliary movement of respiratory cells.
Although the infection rate of men and women is similar, men have a much higher mortality rate than women. Scientists point to the fact that females have two X chromosomes as one of the factors explaining this discrepancy.
The X chromosome is much larger than the Y chromosome. While the X chromosome has 1,150 genes for protein production, the Y chromosome only has around 60 to 70.
“The protein by which viruses such as coronavirus are sensed is encoded on the X chromosome,” says Philip Goulder, a professor of immunology at Oxford University. “As a result, this protein is expressed at twice the dose on many immune cells in females compared to males, and the immune response to coronavirus is therefore amplified in females.”
In the case of diseases involving X chromosomes, women may be less affected because they have two X chromosomes, whereas men have one X and one Y chromosome.
According to Akiko Iwasaki, a Yale professor of immunobiology, the female sex hormones estrogen and progesterone, also play a role in promoting immune responses and reducing inflammation, respectively.
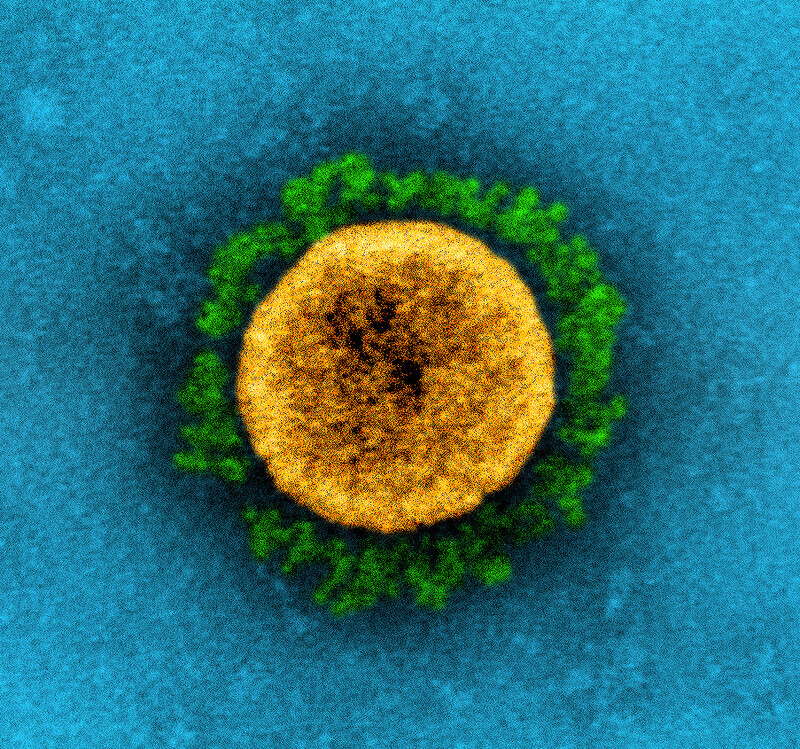
Moreover, the correlation between COVID-19 and blood types is yet another factor that scientists are paying attention to. According to various studies conducted in China and Europe, it has been shown that the most vulnerable blood type to COVID-19 is blood type A while the least vulnerable is type O. Researchers at Harvard Medical School have published a study that shows that the COVID-19 virus binds better to cells of people with blood type A. Moreover, recently, British researchers have published a study on a protein that results in severe COVID-19 symptoms to support this conclusion.
![The receptor-binding domain of the COVID-19 virus adheres to the cells of people with blood type A better than other blood groups. [courtesy of Blood Adv. 2021 Mar 9; 5(5): 1305–1309]](https://flexible.img.hani.co.kr/flexible/normal/640/556/imgdb/original/2022/0329/9816485401011872.jpg)
The most common symptoms among confirmed COVID-19 patients are fever, headache, cough, and sore throat. This has remained almost unchanged throughout the various mutations of the virus. However, the sequence of the symptoms has changed.
When COVID-19 first appeared, the typical symptoms started with a fever, followed by coughing and muscle pain, followed by nausea, vomiting and diarrhea.
However, in the current dominant variant, Omicron, the onset of symptoms starts with a sore throat and progresses in the order of coughing, nasal congestion and finally, fever. Those infected usually experience a sore throat at first and coughing starts after a day or so.
Symptoms such as loss of taste or smell, which were more extreme with the Delta variant, have become less prominent among those infected with Omicron. Overall, patients have exhibited more symptoms similar to traditional colds such as a runny nose, sore throat and sneezing.
Besides symptoms while being sick, another major issue regarding this virus is the aftereffects, now referred to as “long COVID.” This refers to the long-term persistence of some symptoms even following the completion of treatment. In general, any case in which the aftereffects last more than 2 months is considered “long COVID.”
According to Janet Diaz of the World Health Organization, the three most common aftereffects are shortness of breath, cognitive impairment, and fatigue. However, it’s important to bear in mind that there are actually more than 200 reported symptoms among those suffering from long COVID
Researchers in the US followed 200 confirmed patients suffering from COVID-19 for 2-3 months and identified four major factors that lead to prolonged symptoms. The first is the level of the virus in the blood at the beginning of the infection. People with higher virus levels in the early stages of infection were more likely to experience long-term aftereffects. The second case was when the dormant Epstein-Barr virus was reactivated, and the third case was related to people who had Type 2 diabetes. The Epstein-Barr virus is a type of herpesvirus that is often transmitted in childhood and often goes undetected for years.
Fourth is the presence of specific autoantibodies, antibodies produced by the immune system that are directed against one or more of the individual's own proteins. Our body's immune system usually does not make antibodies to target substances within our own bodies, but in some cases, it creates antibodies that attack the body, which can lead to various autoimmune diseases. The researchers found that the most influential factor among the four factors was autoantibodies, found in two-thirds of people suffering from long COVID.
By Kwak No-pil, senior staff writer
Please direct questions or comments to [english@hani.co.kr]

Editorial・opinion
![[Column] When ‘fairness’ means hate and violence [Column] When ‘fairness’ means hate and violence](https://flexible.img.hani.co.kr/flexible/normal/500/300/imgdb/original/2024/0516/7417158465908824.jpg) [Column] When ‘fairness’ means hate and violence
[Column] When ‘fairness’ means hate and violence![[Editorial] Yoon must stop abusing authority to shield himself from investigation [Editorial] Yoon must stop abusing authority to shield himself from investigation](https://flexible.img.hani.co.kr/flexible/normal/500/300/imgdb/original/2024/0516/4417158464854198.jpg) [Editorial] Yoon must stop abusing authority to shield himself from investigation
[Editorial] Yoon must stop abusing authority to shield himself from investigation- [Column] US troop withdrawal from Korea could be the Acheson Line all over
- [Column] How to win back readers who’ve turned to YouTube for news
- [Column] Welcome to the president’s pity party
- [Editorial] Korea must respond firmly to Japan’s attempt to usurp Line
- [Editorial] Transfers of prosecutors investigating Korea’s first lady send chilling message
- [Column] Will Seoul’s ties with Moscow really recover on their own?
- [Column] Samsung’s ‘lost decade’ and Lee Jae-yong’s mismatched chopsticks
- [Correspondent’s column] The real reason the US is worried about Chinese ‘overcapacity’
Most viewed articles
- 1[Column] US troop withdrawal from Korea could be the Acheson Line all over
- 2China calls US tariffs ‘madness,’ warns of full-on trade conflict
- 3[Column] When ‘fairness’ means hate and violence
- 4Could Korea’s Naver lose control of Line to Japan?
- 5[Editorial] Yoon must stop abusing authority to shield himself from investigation
- 6Naver’s union calls for action from government over possible Japanese buyout of Line
- 7Several victims of Jeju Massacre still remain unaccounted for
- 8The quest to rediscover Jeju’s lost towns and villages
- 9Self-driving buses, taxis to hit roads in Seoul in October
- 10A Korean production studio may have made your favorite show – even if you don’t watch K-dramas