hankyoreh
Links to other country sites 다른 나라 사이트 링크
Vaccine won’t completely vanquish COVID-19, experts say
Even if a COVID-19 vaccine is developed, the disease is unlikely to be completely vanquished, and there’s no guarantee that the vaccine will be more effective than wearing masks, health experts say.
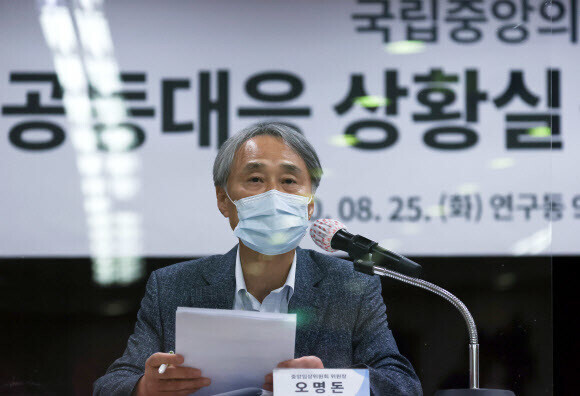
“We won’t have a COVID-19 vaccine until next spring at the earliest, which means waiting for at least eight more months. Though we’re eagerly looking forward to a vaccine, we can’t assume that it will lower the fatality rate or completely prevent the disease,” said Oh Myoung-don, a professor of infectious diseases at the Seoul National University (SNU) College of Medicine, during a press conference at the National Medical Center in downtown Seoul on Aug. 25.
“There’s no guarantee that a vaccine would be more effective at preventing infection than the face masks we’re wearing right now,” added Oh, who also chairs the central clinical committee for emerging infectious diseases at the National Medical Center. The committee is composed of physicians in charge of treating COVID-19.
“Vaccines for respiratory diseases generally don’t obtain the complete effectiveness of other vaccines,” Oh said, explaining his predictions. The parts of the respiratory tract that are infiltrated by SARS-CoV-2 and similar viruses — including the mucous membranes of the airway and the nasal cavity — are on the outside of the body. But the antibodies whose production is triggered by the vaccine can’t leave the body, creating limitations on preventing respiratory diseases. For such reasons, Oh explained, “the US Food and Drug Administration’s requirement for approving a COVID-19 vaccine is 50% effectiveness at preventing the disease, and the flu vaccine has about a 50% chance of preventing infection.”
“Even if a vaccine is developed, that might not be enough to bring the pandemic to an end. For the moment, following personal disease control guidelines — wearing masks, social distancing, and washing hands — is bound to be more effective at preventing infection than any vaccine,” Oh emphasized. While the vaccine will likely reduce COVID-19’s spread and severity to some extent, in other words, it’s much more important to find a balance between daily routines and disease control.
Importance of taking precautions in everyday activitiesOh also urged people to take precautions in everyday activities that are susceptible to infection, such as conversation, singing, and strenuous exercise. “When we breathe through our mouth, the virus goes directly into the lungs, which makes it more likely that we’ll be infected and contract severe pneumonia. Wearing masks is important, but we also need to watch out for breathing through the mouth,” he said.
When asked whether the authorities need to elevate the country’s social distancing regimen to Level 3, Oh said, “That decision should be made carefully in light of the social and economic consequences. Lockdowns aren’t a long-term solution for preventing the spread [of COVID].”
In recommendations for treating COVID-19 released on Tuesday, the central clinical committee said that the only medications recognized as being effective were remdesivir, which can mitigate early symptoms, and dexamethasone, which can reduce the fatality rate. Remdesivir is a medication developed to treat hepatitis C, while dexamethasone is designed to treat allergies and inflammations.
Oh also said the committee had decided it would no longer recommend the therapeutic use of Kaletra or chloroquine, citing their lack of medical benefits. Chloroquine, a malaria medication, and Kaletra, an AIDS medication, were used in the early phase of Korea’s COVID-19 outbreak.
The committee also said that young COVID-19 patients without chronic conditions don’t need antivirus treatments and recommended that such treatments mostly be considered for elderly patients with chronic conditions who have a severe case of the disease.
By Kim Mi-na, staff reporter
Please direct comments or questions to [english@hani.co.kr]
Editorial・opinion
![[Column] Samsung’s ‘lost decade’ and Lee Jae-yong’s mismatched chopsticks [Column] Samsung’s ‘lost decade’ and Lee Jae-yong’s mismatched chopsticks](https://flexible.img.hani.co.kr/flexible/normal/500/300/imgdb/original/2024/0512/3017154788490114.jpg) [Column] Samsung’s ‘lost decade’ and Lee Jae-yong’s mismatched chopsticks
[Column] Samsung’s ‘lost decade’ and Lee Jae-yong’s mismatched chopsticks![[Correspondent’s column] The real reason the US is worried about Chinese ‘overcapacity’ [Correspondent’s column] The real reason the US is worried about Chinese ‘overcapacity’](https://flexible.img.hani.co.kr/flexible/normal/500/300/imgdb/original/2024/0510/5217153290112576.jpg) [Correspondent’s column] The real reason the US is worried about Chinese ‘overcapacity’
[Correspondent’s column] The real reason the US is worried about Chinese ‘overcapacity’- [Editorial] Yoon’s gesture at communication only highlights his reluctance to change
- [Editorial] Perilous stakes of Trump’s rhetoric around US troop pullout from Korea
- [Guest essay] Preventing Korean Peninsula from becoming front line of new cold war
- [Column] The state is back — but is it in business?
- [Column] Life on our Trisolaris
- [Editorial] Penalties for airing allegations against Korea’s first lady endanger free press
- [Editorial] Yoon must halt procurement of SM-3 interceptor missiles
- [Guest essay] Maybe Korea’s rapid population decline is an opportunity, not a crisis
Most viewed articles
- 1[Column] Samsung’s ‘lost decade’ and Lee Jae-yong’s mismatched chopsticks
- 2[Correspondent’s column] The real reason the US is worried about Chinese ‘overcapacity’
- 3[Book review] Who said Asians can’t make some good trouble?
- 4Seoul’s plan to adopt SM-3 missiles is like wanting a sledgehammer to catch a fly
- 5Behind bellicose bluster, N. Korea is turning airfields into greenhouse farms
- 6[Editorial] Human trafficking in S. Korea
- 7Report documents instances of lonely deaths in South Korean society
- 8[Column] “Hoesik” as ritual of hierarchical obedience
- 9Yoon’s broken-compass diplomacy is steering Korea into serving US, Japanese interests
- 10In Yoon’s Korea, a government ‘of, by and for prosecutors,’ says civic group